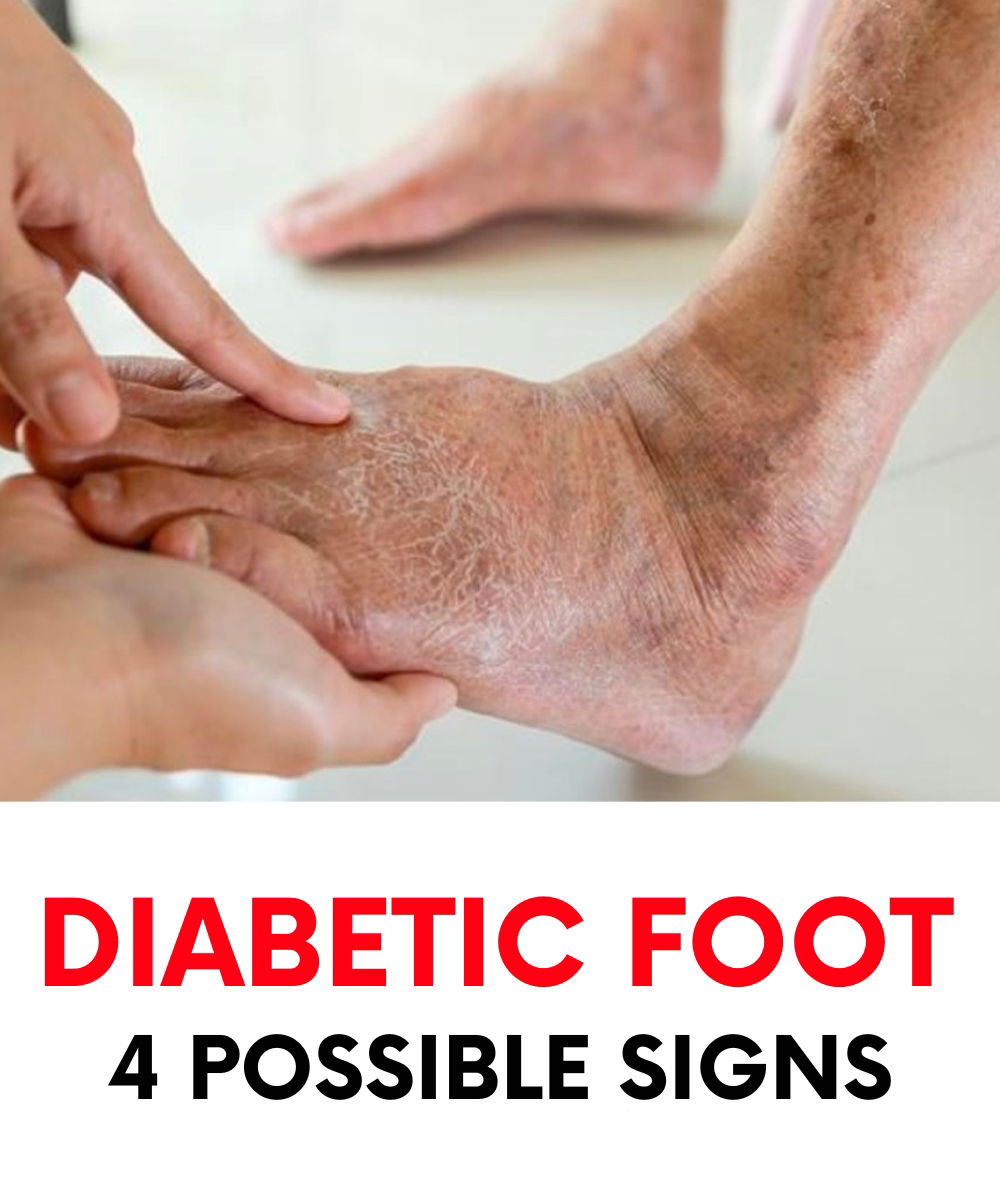
Diabetic foot is a potentially severe consequence of diabetes mellitus that often appears in the form of ulcers or sores on the feet, particularly ones that heal very slowly or not at all.
If you live with diabetes, it’s essential to regularly inspect your feet, between your toes, and along the soles.
Those who have had diabetes for many years, particularly type 1 diabetes, should pay extra attention to their lower limbs.
Feet are far from the heart and often the first to suffer from poor circulation, a common result of long-term diabetes. The condition affects blood flow, reducing the amount of oxygen reaching tissues in the lower body.
Over time, this lack of oxygen and nourishment can cause tissue damage and even necrosis—the death of body tissue.

What Is Diabetic Foot?
“Diabetic foot” describes a disabling condition involving structural and functional changes in the foot and ankle.
It usually stems from two main problems: nerve damage (neuropathy) and reduced blood flow due to artery blockages (ischemia).
Based on the underlying cause, diabetic foot is classified into two types:
- Neuropathic diabetic foot: This form is the result of nerve damage due to consistently high blood sugar levels. It affects sensory, motor, and autonomic nerves, leading to decreased sensation and altered foot structure. Without proper feeling in the feet, individuals are more likely to develop ulcers, especially on pressure points like the soles.

- Neuroischemic diabetic foot: This condition results from poor circulation due to narrowed or blocked arteries. It significantly reduces blood supply to the foot, making tissues more vulnerable to injury, infection, and gangrene.
Why Does Diabetic Foot Develop?
The root causes of diabetic foot lie in the long-term effects of diabetes, primarily nerve damage and compromised circulation.
In type 1 diabetes, the immune system mistakenly attacks insulin-producing cells in the pancreas, causing blood sugar levels to spike.
Without proper insulin management, this surplus glucose damages blood vessels and nerves, particularly in the legs and feet.
Ulcers and blisters tend to form on weight-bearing areas such as the balls of the feet and between the toes. If ignored, these wounds can deepen and allow infection to spread, possibly requiring aggressive treatments.

Early Warning Signs
Diabetic foot often presents with subtle symptoms that shouldn’t be ignored. These include:
- Unusual warmth in one foot
- Numbness or decreased ability to feel heat, touch, or pain
- Tingling or pins-and-needles sensations
- Open wounds, cuts, or sores that heal slowly
Treatment and Prevention
Preventing injury is the cornerstone of diabetic foot care. Daily inspection of the feet is essential—use a mirror or ask someone to help if needed.
Any wound, even a minor one, should be cleaned and monitored closely to avoid infection.
In cases where tissue damage becomes severe, amputation might become necessary. This is a last resort and highlights the importance of early intervention and prevention.

To avoid reaching this stage, adopt proactive habits:
- Keep your feet clean and dry
- Wear well-fitting shoes made of breathable materials
- Choose socks made from natural fibers
- Avoid walking barefoot or wearing tight footwear
- Don’t self-treat foot issues—see a specialist, especially for nail care
Above all, manage your diabetes carefully. Follow your treatment plan, take medications as prescribed, and have regular check-ups. Your diligence can significantly reduce the risk of developing diabetic foot and protect your overall well-being.